Why Is The Battelle N95 Mask Sterilization Contract So Expensive?
Jim here.
Long time readers of the blog know that whenever I hear something about Battelle, my spidey senses go on full alert. Suffice it to say that the Battelle facility in West Jefferson, Ohio is one of only a few facilities on the planet that has both the expertise and the equipment to produce something like, say, a fully weaponized anthrax powder. So I’ve been going on alert the last few days as word has come out on Battelle’s process for sterilizing used N95 masks for re-use. West Jefferson is just outside Columbus, so I had a false alarm on Marcy’s post earlier today about the Washington Post needing to go to Columbus, but she wasn’t discussing Battelle.
Don’t get me wrong. I am fully in favor of anything that can be done to provide safe PPE to those on the front lines of the COVID-19 pandemic response. Finding safe ways to re-use these masks has to be one of the many approaches we must rely on while the masks are in such short supply. But when I finally started digging deeper into what is going on with the contract that the Defense Logistics Agency awarded to Battelle for this process, I was staggered by the total cost compared to what looks, on the surface, to be a straightforward, inexpensive already proven approach.
On April 13, the Department of Defense announced a $415 million contract to Battelle for N95 mask sterilization:
The Department of Defense’s Defense Logistics Agency, on behalf of the Department of Health & Human Services (HHS), has awarded a $415 million contract for 60 Battelle Memorial Institute Critical Care Decontamination Systems (CCDS), that can decontaminate up to 80,000 used N95 respirators per system per day, enabling mask reuse up to 20 times.
Spearheaded by the Department’s Joint Acquisition Task Force, six units have already been delivered to locations including two to New York, and one each to Columbus, Ohio, Boston, Chicago and Tacoma, providing the ability to sterilize 3.4 million masks a week, reducing the need for new masks by the same number.
All 60 systems will be available by early May for prioritization and distribution by FEMA and HHS. Once all are delivered, these 60 units will allow 4.8 million masks to be sterilized per day, almost 34 million per week.
‘I remain extremely proud of the selfless efforts of Department of Defense personnel who continue to do everything they can to help provide medical masks, test kits, medicine and meals to support America’s military, medical, emergency services and law enforcement professionals who are on the front lines and need them most,’ said Under Secretary of Defense Ellen Lord.
This procurement includes a service contract to cover operations and maintenance.
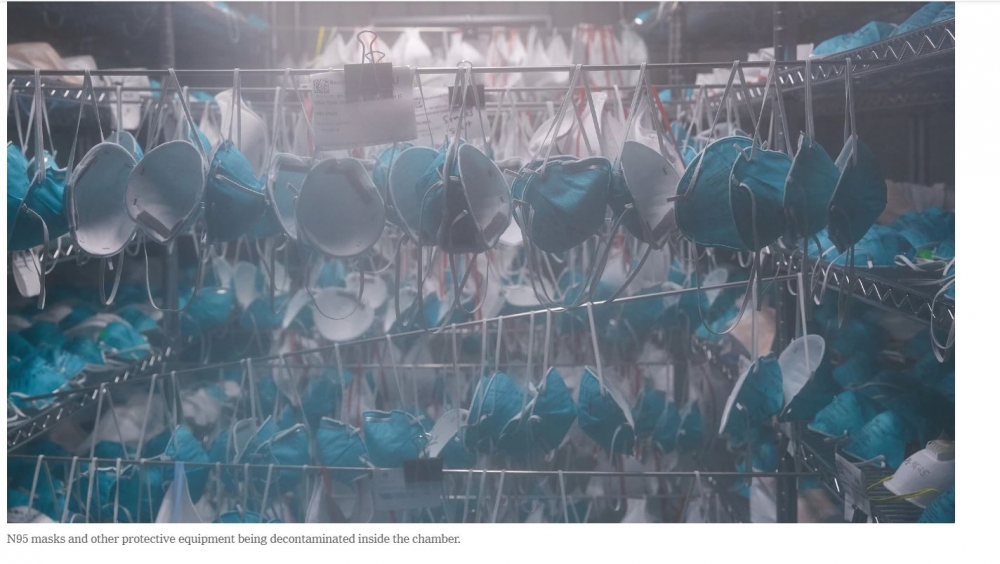
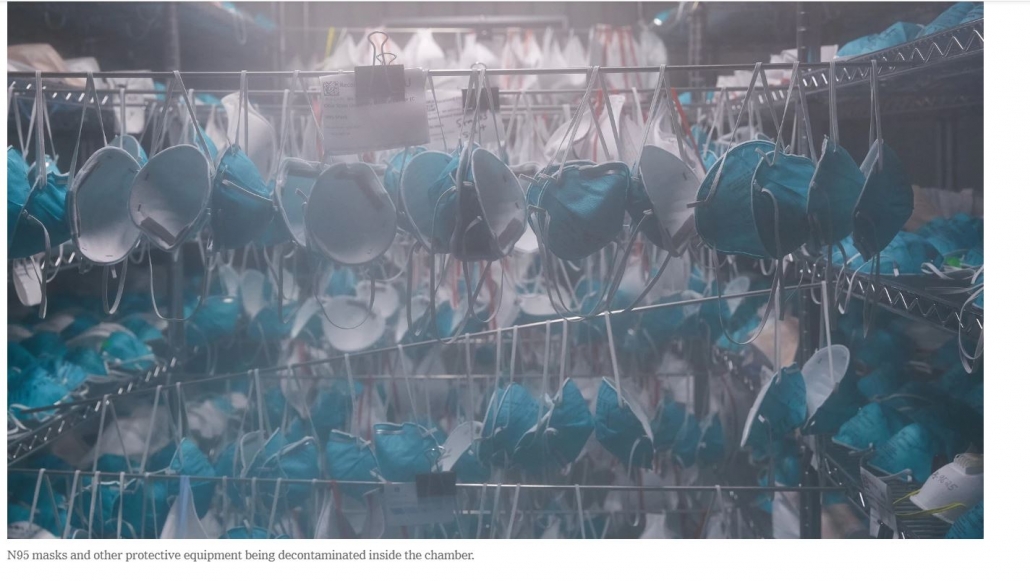
A couple of days earlier, on April 11, the New York Times visited Battelle and provided a photoessay on the Battelle process for sterilization. Here is a Times photo of masks hanging in one of the decontamination units. This photo is also the featured image for the post:
One thing that jumps out immediately is to notice that standard food/medical grade shelving is used in the unit. So at least that part isn’t very expensive. I am disturbed, though, by the “extra” rods between shelves that have masks hanging in a way that we can see multiple pairs of them closely nested, raising concern about circulation of the vapor used in the sterilization process. Just below the photo, the Times notes that workers take “care to avoid overlapping”. Okay, then, but I’m still nervous about those that look nested.
The sterilization process itself is carried out by hydrogen peroxide vapor (HPV). Of course, safety dictates that the chamber in which the masks are exposed to the vapor is perfectly sealed as vapors escaping would be toxic to the staff working around the chamber. Technology to inactivate the peroxide in the exhaust stream from the chamber is known, off the shelf technology and would be a part of the air handling for the chamber. Hydrogen peroxide itself is very inexpensive and is produced in bulk by the chemical industry.
Battelle already validated the process under a contract from FDA, with the final report issued in July of 2016 (thanks, Obama!). Here’s a partial screengrab from the report with a photo of the simple machine used to generate the HPV (gratuitous anthrax mention included for grins):
Sure enough, the Times found a very similar machine when they were at Battelle:
This is not a very complicated piece of machinery. I’m not sure of the full retail price, but I found a used “as is” listing for $4500. I’d be surprised if these are costing Battelle more than $20,000 per unit.
And the “chambers”? They’re shipping containers. Again, from the Times photos:
Also visible in this photo is very standard-looking air handling equipment.
So, making 60 units out of shipping containers, outfitting them with an HPV generator and air handling equipment doesn’t look very expensive to me at all when compared to the total value of the contract. It’s very hard to estimate more than $10-15 million in materials costs for 60 units.
The Times article provides an accessible description of the sterilization process. Here’s what happens in the chamber:
A contraption known as a vapor phase hydrogen peroxide generator, which looks like a washing machine with two hoses, is then used to circulate the colorless gas into and out of the room. During the first four hours, workers increase the humidity inside the chamber, causing the hydrogen peroxide to collect as condensation on the masks, neutralizing the coronavirus and other contaminants.
Over the next four hours, the gas is flushed out of the room. The teams then re-enter the chamber to inspect the masks and conduct spot tests for harmful levels of residual hydrogen peroxide. They then confirm that chemical indicator cards placed throughout the chamber have changed color — the sign of a successful decontamination.
The process itself is very labor intensive, although the masks are inside the chamber for what looks like 8 hours in between bouts of activity. The masks have to be handled and inspected both before and after the sterilization procedure.
Is the labor the reason the contract costs so much? A key missing piece of information is just how long the contract lasts. Recall that the DOD press release indicates that Battelle is providing the labor for the process along with maintenance of the chambers.
After a bit of digging, I found a few more details. Here is information from a Defense News post that is dated April 13 in its URL:
Battelle has already set up two machines in the New York City area, as well as one each in Chicago, Illinois; Tacoma, Washington; Columbus, Ohio; and in the suburbs of Boston, Massachusetts. A solicitation on the organization’s website, found by the Boston Globe, says the group anticipates a need of at least 2,300 workers for 100 sites — or 23 staff per site, which is expected to run 24 hours a day. The $20 per hour job is expected to last at least four weeks.
“We are anticipating a surge over the next two months,” the solicitation read.
Let’s be generous here and extend that two month surge to a full year. If there are 2300 workers each making $20 an hour for a year, I calculate a little under $96 million in direct costs. Being generous again, travel expenses (Battelle in their solicitation mentioned the employees may need to move among sites), benefits, and overtime may bring total personnel costs close to $200 million.
My gut feeling here is that Battelle stands to make quite a bit of money off this contract, even if they run full-out with these chambers for a full year.
But rest easy, citizens. Battelle plans to provide the sterilization service free of charge for those submitting masks and other equipment for processing.