Rikers and Roosevelt: The Uncontrolled Human Experiment Occurring with Essential Workers (and Their Wards)
In the several weeks since much (though not all) of the country has been shut down, an uncontrolled human experiment with the country’s essential workers has been occurring.
I say that because those people still required to work — especially medical care workers, nursing home workers (and their clients), prison guards (and prisoners), cops, meatpackers, grocery store workers, warehouse workers, public transit workers, and sailors and other service members — have all been asked to work with a very limited test and tracking regime in place to limit spread among co-workers, wards, and their communities.
There’s inconsistent public data about how closely the federal government is tracking these communities (they’re obviously tracking the military, and after an initial attempt to hide the numbers, have provided skeleton baseline numbers; they’re reportedly not tracking nursing homes). So what has happened in these populations cannot be described with precision yet. But there is public reporting on how seriously affected each of these groups are — and whether, and when, their employers took appropriate protective measures. Thus far, the anecdotal reports show that some individual institutions have been more successful than others at preventing mass infection, whereas certain kinds of worksites — prisons and ships — will have much less success controlling an outbreak given existing tools.
These professions are where spread is happening even with shutdowns (though some, like meatpackers, are often located in areas more likely to have shut down late or not at all). Thus, amid the debate about when we can reopen the economy, what happened to workers and their wards in these professions provide lessons about what protections have to be in place before any place can open up, how widespread COVID might get amid populations that social distance but don’t stay home, and what pitfalls are likely once we do open up.
Along the way, a lot of people have died.
Update: Elizabeth Warren and Ro Khanna have called for a Workers Bill of Rights that includes–but then adds to–a lot of the protections included in this discussion.
Medical care workers
In a recent presser, Trump claimed that the federal government eventually will figure out how many medical workers have contracted COVID-19 (though I suspect that number won’t be made public until after the election). But it hasn’t done so yet. Buzzfeed collected what was publicly available and found that key states, including New York, Louisiana, and Michigan, are not tracking this number either yet.
Buzzfeed tallied 5,400 cases in those states that are counting it, which would work out to be 1% of the cases on the day of the story (though because some of the most important states aren’t counting this, it must be a higher percentage of national cases).
At least 5,400 nurses, doctors, and other health care workers responding to the coronavirus outbreak in the United States have been infected by the disease, and dozens have died, according to a BuzzFeed News review of data reported by every state and Washington, DC. However, the true number is undoubtedly much higher, due to inconsistent testing and tracking.
[snip]
As of Thursday afternoon, 12 states reported health care worker infections: Alabama (393), Arkansas (158), California (1,651), Idaho (143), Maine (97), New Hampshire (241), Ohio (1,137), Oklahoma (229), Oregon (153), Pennsylvania (850), Rhode Island (257), and West Virginia (76). Additionally, Washington, DC (29) and Hawaii (15) reported infections at a specific hospital, not state or territory-wide. On Friday afternoon, Kentucky reported 129 health care worker infections.
In Ohio and New Hampshire, health care worker infections represented more than 20% of total confirmed cases in the state. It’s unclear if this is due to health care workers having greater access to testing there compared to other states, or something else, but it highlights the dangers these workers face. In the other states that broke out data on health care workers, rates ranged from a low of nearly 5% in Pennsylvania up to 17% in Maine and Rhode Island.
Some other states are trying to collect this information but not yet sharing it publicly, with officials citing reporting holes in their data.
[snip]
And in at least nine states, infection rates among health care workers are not being tracked at all. That includes New York and Louisiana, two of the worst-hit states by the outbreak, where officials said they aren’t specifically collecting this information. In Michigan, another hard-hit state, 2,200 health care workers have reportedly been infected, yet the state itself is not tracking infections. (Because the reporting on these cases did not come from the state itself, BuzzFeed News is not including them in its total.) Fourteen states do not make these statistics publicly available and did not respond to questions from BuzzFeed News as to its collection.
As that story noted, these numbers are unreliable both because health care workers may have better access to tests, but are, in many cases, being discouraged from taking them. And workers are so overwhelmed right now it may undermine record-keeping.
Plus, there are significant discrepancies from hospital to hospital regarding how much PPE is available to workers, not to mention how overwhelmed the individual hospitals are. Hospitals that succeed at keeping infection rates low will have lessons to offer on what might successfully limit transmission among workers who are highly trained in doing so, lessons that would be of use in professions not normally trained to prevent contagion.
Nursing homes
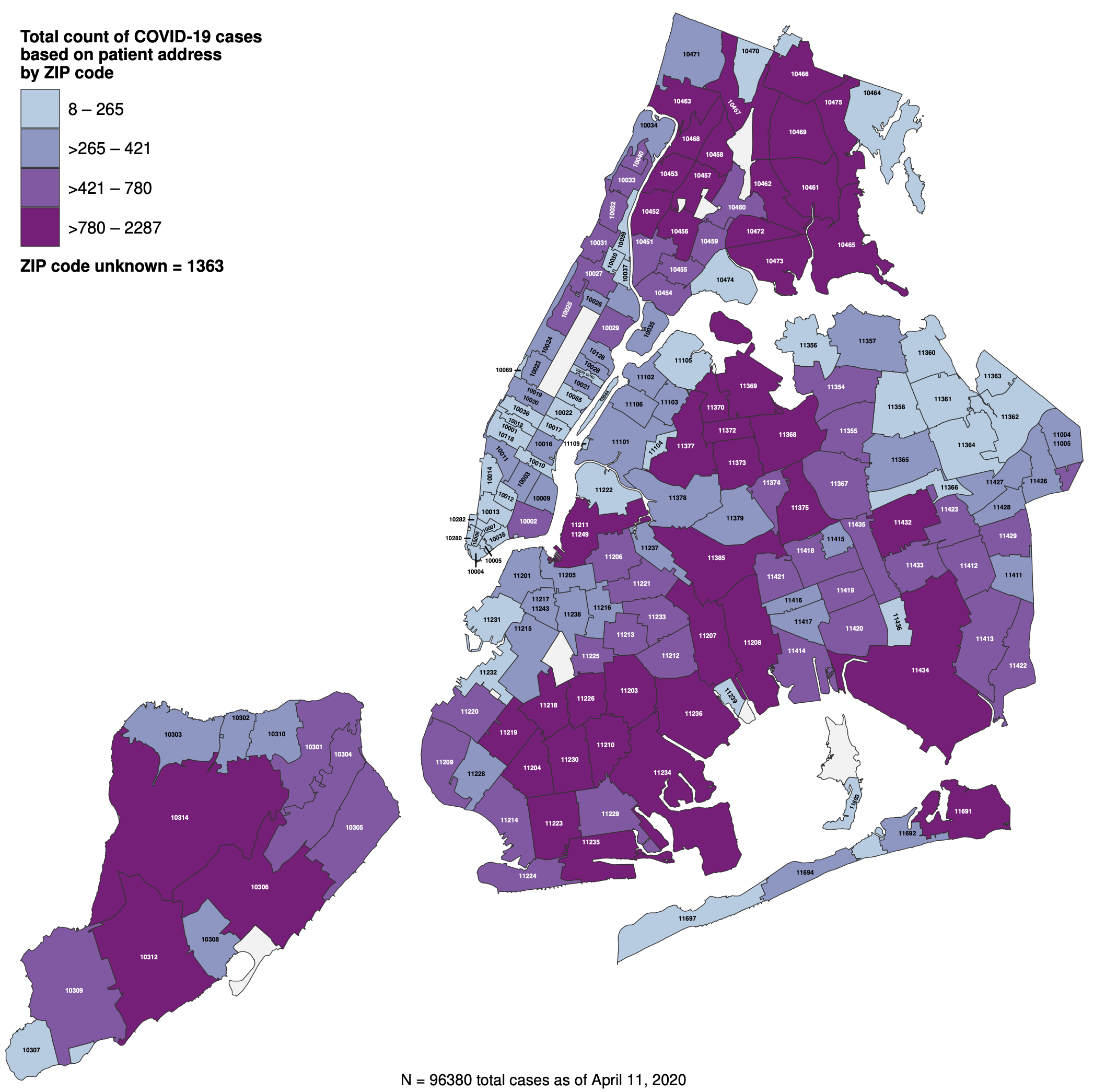
Nursing homes are another obvious cluster — so much so that they may make up a huge proportion of what we’re seeing in non-crisis localities (as is the case in my own county). Like medical care workers, there’s not an official count; indeed, some states (especially Florida) are affirmatively hiding how badly nursing homes are being affected and ending efforts to count clusters among seniors. Nevertheless, NBC found over 2,200 deaths in the states that do count such things, representing a huge spike since March 30 (which would suggest nursing homes are where the virus has continued to spread since states and localities that have shut down).
Nearly 2,500 long-term care facilities in 36 states are battling coronavirus cases, according to data gathered by NBC News from state agencies, an explosive increase of 522 percent compared to a federal tally just 10 days ago.
The total dwarfs the last federal estimate on March 30 — based on “informal outreach” to state health departments — that more than 400 nursing homes had at least one case of the virus.
[snip]
Thirty-six states reported a total 2,489 long-term care facilities with COVID-19 cases.
The toll of these outbreaks is growing. NBC News tallied 2,246 deaths associated with long-term care facilities, based on responses from 24 states. This, too, is an undercount; about half of all states said they could not provide data on nursing home deaths, or declined to do so. Some states said they do not track these deaths at all.
As with the county of medical workers, key states like Michigan and Florida are tracking neither which facilities have clusters nor how many deaths there are. New York is tracking this statistic.
Nearly 60 percent of the deaths tallied by NBC News occurred in New York, where more than 1,300 residents of nursing homes and assisted living facilities have died, according to the state health department.
That would represent around 18% of the deaths New York had recorded by April 9, the day before NBC published.
And these data generally only count residents affected, not the workers who might spread the virus outside of the facilities.
As Andy Slavitt explained in his Rachel Maddow appearance to discuss this data, one of the key lessons in the outbreaks at nursing homes and other assisted living facilities (though the lesson applies to all these “essential” professions) is the differential impact. Some facilities have succeeded in containing the virus, others have failed to contain known outbreaks. Those that have succeeded have lessons to offer about how to deal with this virus effectively.
The way this will get fixed — this is not to embarrass anybody — but the way this will get fixed is there are nursing homes that are doing it right. And the nursing homes that are doing it right can give guidance to the nursing homes that are doing it wrong. We don’t have enough time to go back to the drawing board and create new regulations — I wish we did. But in the middle of a crisis, I’d get them all on the phone, we’d be sharing best practices, we’d be publishing them, and we’d be slowly and slowly taking down infection rates. And for those that couldn’t do it, we would be moving people into facilities that could.
Nursing homes are, along with prisons, probably the hardest population to keep safe from COVID and there are aspects of both (the underlying health problems and the immobility and close quarters of the facilities) that are impossible to eliminate. But that means the lessons learned here — particularly the lessons learned about how to keep the workers safe (and therefore to prevent intra- and extra-facility spread through them), would be critical to share not just within the nursing home industry, but more generally with businesses as they think about reopening down the road.
Update: According to the AP, Louisiana has now stopped providing details on infections in nursing homes.
Prisons
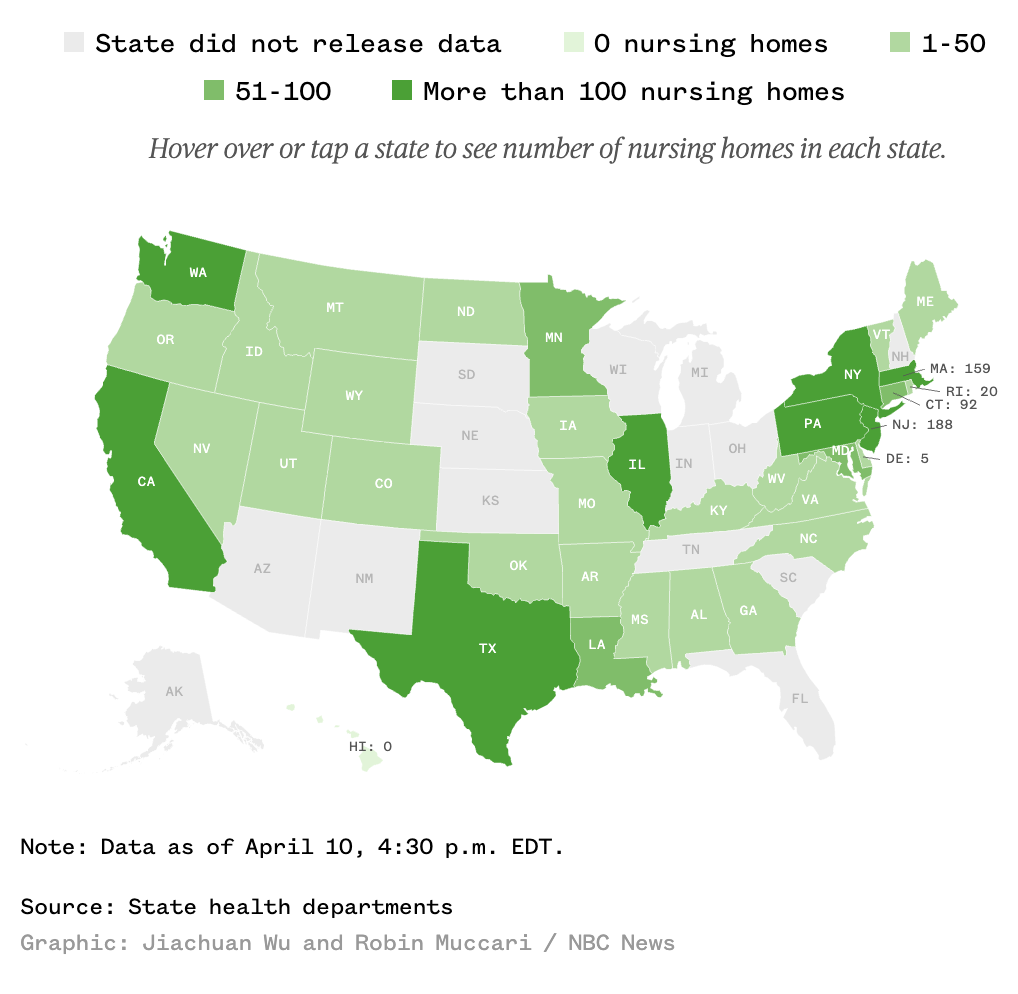
Immediately after the impact of COVID became clear, prisoner advocates started calling for decarceration to alleviate crowding and remove the most vulnerable prisoners, where appropriate, from prison. Ohio’s Republican Governor Mike DeWine has even laid out the epidemiological reason to take such measures (that is, the obvious conservative case to release as many prisoners as possible), and Oklahoma’s Republican Governor Kevin Stitt (who was otherwise tardy in taking measures to stop the spread), is preparing to commute the sentences of 452 people to empty the prisons. Even Bill Barr has pushed for prisoner releases. His efforts risked disproportionately help white prisoners, but because BOP is now prioritizing those facilities already affected by an outbreak — meaning they’re acting reactively, not proactively — that has not yet been the practice. That said, Federal policies on releases are changing day-to-day, with some prisoners cleared for release but then continued to be held.
BOP has an official tracking number — though they’re not testing everyone. So in the prisons where there’s a real cluster, the numbers are likely far higher. For example, at Elkton, OH which BOP says has 13 inmates infected, 37 prisoners have been hospitalized with symptoms and another 71 are in isolation. At Oakdale, LA — where the first BOP death occurred and one of the hardest hit — BOP claims 40 inmates have tested positive, but at least another 56 have been hospitalized with severe symptoms and 575 are quarantined.
With regards to state and county prisons and jails, however, those counts are often still spottier — and potentially far more urgent given greater overcrowding. UCLA Law has put together a database that tries to track all the known cases (though, as one example of its limits, it only shows New York’s case statewide).
Nowhere is the spread of COVID in prison more concerning than in urban jails. NY City’s Rikers, which as of Wednesday had over 700 infections. 440 of those are staff, meaning the 287 count for inmates testing positive is surely a significant undercount. Nevertheless, that undercount shows that 6.6 percent of Rikers prisoners have tested positive, a rate seven times higher than New York as a whole. Unfortunately, this all happened at a time when Andrew Cuomo and others were trying to reverse recent measures to decarcerate New York, and Cuomo has lagged some of his Republican counterparts in his efforts to cut prison populations and so limit the spread there. Cook County, IL’s jail has 304 positive detainees and 174 correctional officers who tested positive, similar or slightly higher rates than Rikers. This week a judge ordered the Cook County Sheriff to provide soap and sanitizer to prisoners, test those exhibiting symptoms, and provide PPE to those quarantining because of exposure, but stopped short of ordering the jail to release prisoners.
Thus far, that’s what the emphasis has been: emptying the jails. That’s a welcome approach, as a number people who shouldn’t be in jail or prison (or immigration detention) have been released. It’s not clear that prisons have solved the problem of COVID and efforts to do so often end up being inhumane, leaving sick prisoners in solitary and the general population with far less ability to contact their lawyers, to say nothing of family members, which only adds to the panic and confusion for all involved.
One thing that is unclear is whether COVID has spread through guards to the surrounding population, something that — because so many of our prisons are located in rural areas — might be a vector for COVID to spread to the surrounding communities.
These badly affected prisons, however, are going to have an interesting dynamic between guards and prisoners. In Oakdale, for example, there has already been a clash between guards and prisoners. But in other places, the situation has put guards and prisoners on the same side of legal challenges to push for more releases, something that rarely happens in prisons.
No one is going to solve the problem of how to go back to work at prisons. But if you want to see the kind of societal upheaval that might happen if this effort fails, prisons may be your first measure.
Update: Florida has now tasked inmates to make cloth masks for guards, but not for themselves.
Update: Lansing Correctional Facility, in Kansas, also had a riot believed to be COVID-related last week. There are 16 staff and 12 inmates confirmed to have COVID-19.
Cops
Cops interact less directly with COVID patients and often in less enclosed environments than medical care, nursing home, and prison workers, which may make them a better read of what kind of exposure will happen among those who have to interact with a range of the public, but not necessarily a population particularly exposed.
Nevertheless, COVID had spread broadly among the police departments of the bigger cities with COVID spikes, including New York, Detroit (exacerbated by a pancake breakfast attended by a bunch of cops that was an early transmission vector), and Chicago, and known exposure has led significant numbers of cops and other first responders into quarantine, illness, and death (there are other major metros for which reports of exposure among cops is more dated and in smaller numbers). As CNN described it, the toll at the NYPD rivals (though, because of the lasting after-effects of 9/11, could never be counted in the same way) 9/11:
In a department of about 36,000 sworn officers, 7,096 — or 19.6% of the uniformed workforce — were out sick on Friday, according to data issued by the NYPD. Some 2,314 uniformed members and 453 civilian employees have tested positive for Covid-19, and 19 employees have lost their lives as a result of the virus.
The NYPD suffered an incomprehensible 23 losses on 9/11 (hundreds more died in subsequent years from 9/11-related illnesses). It’s devastating to think that the casualties from Covid-19 may soon eclipse this.
IACP and CDC guidance for first responders currently only recommend using PPE when interacting with known or suspected COVID carriers. And this week, the CDC issued new guidance for critical workers (especially including but not limited to first responders) who’ve been exposed that permits returning to work while wearing a mask rather than a full quarantine. This effort was explicitly rolled out in an effort to address staff shortages like those in police departments.
That guidance — which relies on temperature checks rather than testing — hints at where the Trump administration intends to go as it pushes people to return to work. Which is to say, its first effort to get people back to work falls far short of the testing regime most experts say we need to control the spread.
Military
The military initially tried — in the name of national security — to prevent the release of any granular data showing where its cases are. But then William Arkin published a map showing where the 3,000 cases (of which 2,031 were uniformed military on Friday) were. That same Friday report showed 13 total deaths.
I’m particularly interested in the clusters at bases in Anchorage and Honolulu in states not otherwise heavily impacted by the virus. It suggests that the military may be a vector to spread to unaffected places.
That is a rate of infection that is higher than the US as a whole (which likely stems, at least in part, to greater access to testing), but with a mortality rate significantly lower than the overall rate.
The new count puts the department’s death rate at 0.4 percent, versus the overall U.S. mortality rate of 3 percent.
[snip]
The military’s infection rate now stands at 971-per-million, compared with the latest Centers for Disease Control and Prevention numbers, which shows 1,307-per-million U.S. residents having contracted coronavirus, or about 0.1 percent of U.S. residents.
Nowhere has the challenge of COVID been more dramatic, however, than on the USS Theodore Roosevelt. As the scandal over Captain Theodore Crozier’s removal and the ouster of Navy Secretary Thomas Modly has continued, the Navy has continued to test the entire crew of around 4,800. With 92% tested yesterday, 550 tested positive, meaning 12% of those tested, tested positive. That’s a lower rate than the Diamond Princess’ 19% positive rate, but of a younger and presumably far healthier population, during a period with a higher level of awareness of the virus, and among a population more likely to maintain the discipline of social distancing.
Keeping sailors on a ship from infecting each other is a daunting task, but the military has more resources to conduct evacuation and to conduct contract tracing than any private employer this side of Amazon. As other ships and bases face the challenge in the wake of the Roosevelt fiasco, it will be a measure of whether even the military can catch the virus and contact trace before other big clusters arise.
If the military can’t do it, your average small business isn’t going to be able to pull it off.
Update: The sailor who had been moved to the ICU has now passed away from COVID-19.
Transit workers
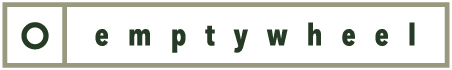
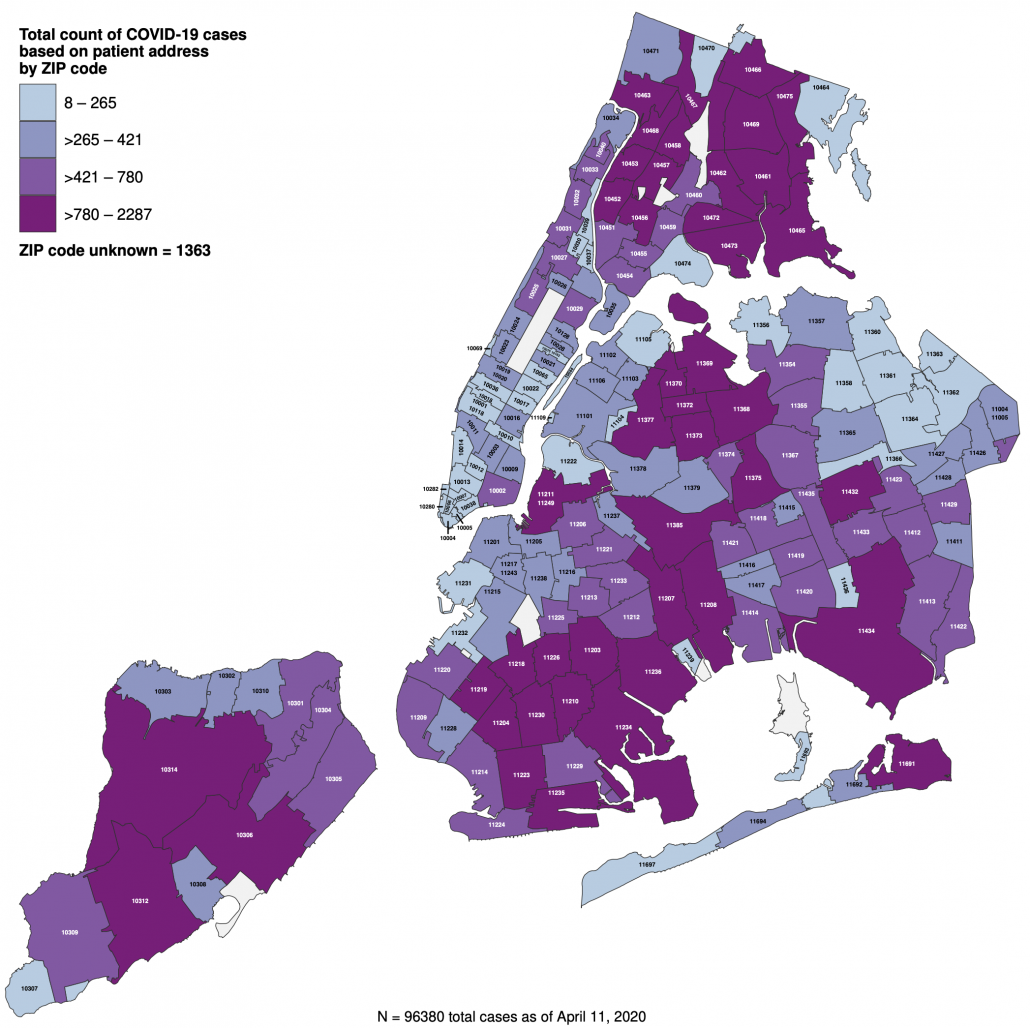
One reason New York has been so badly hit is so many people rely on public transportation. Even NY’s suburbs are among the hardest hit area of the country (with 34,392 cases on Long Island, or 21% of the state’s total), and the outer boroughs, where poverty and continued exposure via “essential” jobs, are hardest impacted by the virus within the city.
That’s why the outbreak on the MTA offers important warnings about the possibility that New York could reopen anytime soon. That’s true not just because of the high levels of infection and death — around 14% of MTA 50,000 employees have either tested positive or are quarantining with symptoms, but also because COVID has led to a shortage of workers which has in turn badly hurt service.
At least 41 transit workers have died, and more than 6,000 more have fallen sick or self-quarantined. Crew shortages have caused over 800 subway delays and forced 40 percent of train trips to be canceled in a single day. On one line the average wait time, usually a few minutes, ballooned to as high as 40 minutes.
[snip]
Still, around 1,500 transit workers have tested positive for the coronavirus, and 5,604 others have self-quarantined because they are showing symptoms of the infection. Absenteeism is up fourfold since the pandemic began, officials say.
If more people were working, this shortag would make it harder for passengers to engage in social distancing themselves (though usage is down 70% for buses and 92% on subways).
While MTA dawdled in imposing protective measures for employees, it now surpasses CDC guidelines, in part by providing masks to all its employees.
Patrick J. Foye, the M.T.A. chairman, who himself tested positive for coronavirus, said the agency initially followed guidance from the World Health Organization and the Centers for Disease Control and Prevention that healthy people did not need to wear face masks.
Mr. Foye said the M.T.A. then decided to go farther than that, before the C.D.C. changed its advice on masks. He said it had already provided 460,000 masks to workers, in addition to thousands of face shields and 2.5 million pairs of gloves.
So long as the stay-at-home order remains in place, this crunch on transit won’t prevent people from working, which if it happens would hit those who can’t afford Uber the hardest. But until NY can find a way to limit the illnesses on transit, there’s no way the city can reopen.
Meatpackers
This week a lot of attention has focused on meatpacking plant. The numbers of people infected aren’t high, on a national level, but they’re shutting down factories that supply a significant percentage of the nation’s meat supply, and often in more rural places that until recently believed they were immune to the virus.
A Tyson-owned meat processing plant that churns out 2% of the US pork supply ground to a halt this week as workers became infected with Covid-19.
And that wasn’t the only meatpacking plant impacted by the spread of the novel coronavirus. JBS USA on March 31 said it hit pause on much of its work at a beef facility in Souderton, Pennsylvania and wouldn’t have it back online until mid-April. National Beef Packing on April 2 temporarily stopped slaughtering cattle at one of its plants in Tama, Iowa after a worker tested positive for the virus.
Perhaps the most notable of those cases is in South Dakota, where a Smithfield pork processing plant first closed for three days, after 80 employees had tested positive, and then today closed indefinitely after that count grew to 293, 8% of the plant’s workers (it’s unclear whether all the worker at the plant have been tested). The cluster is also significant given that those cases make up 40% of the cases in South Dakota, which has not imposed a stay-at-home order. As such, it’s an example of a workplace that, by not managing an outbreak, can significantly impact a community that may have assumed it was immune.
Guidance released by an industry organization dated April 3 noted that the industry wasn’t getting PPE because shortages mean what is available needs to be saved for medical workers, which suggests that even for an industry that recognizes the need (some of these companies also operate in China), they’re not able to provide masks for their workers because the shortage for medical workers hasn’t been solved.
Update: On April 8, the UFCW called for CDC to issue mandatory guidelines that would cover both the union’s grocery store and its food processing workers. It includes employer-provided PPE for the workers.
Businesses and services have had from two weeks to months to try to prepare their workplaces for this crisis — and for none of them has there been any doubt about their essential status. But they’re still not doing some of the basic things that experts say we’ll need more generally to reopen the economy. These workplaces — the ones for which there is some kind of real count — are facing up to 12 to 19% COVID positive rates, even in professions with a strong culture of hygiene (though none of these professions, not even medical workers, can get the testing to confirm those rates). The resulting staffing shortages are causing service shortfalls even beyond the hospital staffs we’ve been working to flatten the curve to accommodate. And for many of these communities, those numbers reflect weeks of stay-at-home orders that limit the sources of new infections.
Trump wants to reopen the economy. But it’s clear from the limited data and anecdotal reporting from essential workplaces that basic things — starting with masks — still aren’t in place to limit workplace exposure.
And again, because these men and women haven’t had the protective equipment or other workplace protections they need, many have needlessly died.




Retail banks, for example, still do not have protections for their staff: masks, gloves, hand sanitizer, cleaning supplies, added windows to reduce spray from breathing, coughing, and sneezing. (Currency, a hybrid textile fabric, tends to hold onto things that touch it.) The local gas station has them.
Yet, staff are expected to show up to work with a happy face. Just as bad, bank systems hiccup – ATMs refuse routine deposits – and customers are required to show up in person to sort out their complaints and basic transactions. Retail banks will be another locus of infection.
The banks I’ve dealt with in the last few years have windows between the tellers and the customers, but the cubicles where they discuss things like loans don’t have anything like that.
(The pharmacy I go to has put in windows also, in the last couple of weeks.)
A pharmacy I go to that is part of a dedicated health/hospital system had masks, gloves, nurse and security guard checking temps at entrance. Large national chain a week later – no gloves, no masks, on any employees.
Here in metro KC, a number of banks have basically closed their lobbies for ordinary transactions when the “stay at home” orders were issued, with customers being sent to either ATMs or driveup windows. No hiccups that I’ve heard about around here.
The message is clearly “what we do is critical, but we’re changing the way we do it to try to keep everyone healthy.”
One of the big frustrations I have with reporting on masks (and other PPE) is the lack of basic estimates on needs and goals for production.
One number I have seen is a Department of HHS estimate that medical workers will need 3.5 billion for a severe event, which presumably we are facing now:
https://www.businessinsider.com/usa-1-percent-3-billion-face-masks-needed-coronavirus-pandemic-2020-3
But that is just medical workers, and doesn’t address all of the other workers (and members of the public). Presumably social workers in nursing homes, parole officers, school cafeteria workers, and whole other universes of people will need huge numbers of masks too.
Typical reporting on masks doesn’t even include this number. For example, this article talks about a 39 million production target, which might sound impressive but doesn’t mention that this represents only about 1% of the expected need. For medical workers only.
https://www.reuters.com/article/us-health-coronavirus-pentagon/pentagon-awarding-contract-to-boost-n95-mask-production-capacity-by-39-million-idUSKCN21T0U8
I have to assume at this point that the White House is doing everything it can to keep this kind of information under wraps to avoid more bad PR, and also to grease the push for an end to restrictions — if people knew how much longer it will take to get masks to the people who need them, they’ll be less likely to support Trump’s push.
And right wingers who are fighting expansions of government involvment in the supply chain will want to avoid public understanding of the need for a massive increase in federal engagement. When 3M says that they hope to be making 50 million a month by the end of June that sounds impressive, until you do the math and see that comes out to only 600 million a year, or 1/6 of the need. Again, only for the estimated need for medical workers.
https://news.3m.com/blog/3m-stories/3m-responds-2019-novel-coronavirus
This is the kind of data that good media outlets ought to be able to investigate and publicize in every single article on PPE they publish. But they don’t seem very interested in providing that kind of context, leaving the White House to operate in a vacuum.
One other facet of the PPE reporting I believe has failed us: the use of past pandemics to predict needs. Neither the administration nor the media seem to grasp THIS IS NOT INFLUENZA. It’s not as bad as measles in terms of transmission but it’s much, much worse than influenza, requiring a different level of production to meet health care workers’ needs let alone what the public needs.
I don’t know whether 3M, as one example, is framing its responses about mask production because it may also be producing other PPE like face shields not used in influenza pandemics.
It’s just so pathetic that hospitals are relying on hobbyists with 3D printers and open source designs to provide additional PPE needed beyond masks.
I agree about the framing, and I think with enough drilling it’s possible to find specialists who are addressing a bunch of these issues.
But the problem is that editors and producers are heavily conditioned to defer to “expert” opinion that is really upper level opinion.
They are so hung up on the framework of filing a story that they have no concept of the value of finding out what the story really is.
This works OK for covering a disaster like a plane crash where the NTSB leadership is well practiced and the issue is narrowly defined. But it completely falls apart today where you have a bunch of posers in charge, and editors and producers who don’t want to work any differently.
Ford Michigan taking matters into their own hands. And assembling by hand, 6 per minute.
https://www.freep.com/story/money/cars/ford/2020/04/06/ford-uaw-make-million-face-shields-nypd-nyfd/2951650001/
Reading this I was wondering if freezing meat might kill the coronavirus;
No not according to this article:
How long can coronaviruses survive in a freezer? Up to two years, warns expert
https://english.alarabiya.net/en/features/2020/03/19/How-long-can-coronaviruses-survive-in-a-freezer-Up-to-two-years-warns-expert
The good news is that cooking the meat normally will kill it.
And then there is that ubiquitous service that is so familiar that it is almost invisible, like air: Postal Service. Traipsing door to door, often with no more than junk mail, they come here with no PPE daily. And they go to all the other places mentioned, too: the nursing home down the street, the grocers, the Naval Stations, etc.
I’ve been trying to keep up with BOP numbers since the end of February, searching through the news and the BOP websites. Prior to April 1 or 2, when their central virus website went up, I could only find under a dozen cases, most of them at Manhattan, and no deaths. I don’t remember the exact initial web site figures, but they weren’t incredibly shocking either in the number of cases, or number of facilities impacted, I think around 25 or so. Since then, the climb has been steep and swift, with new reports of 500+ staff and inmates infected, and 10 deaths, in less than ten days. Its possible that to an extent this is a result of a lack of information coordination prior to the site going up, being corrected in a single week, or it could also be that the spike is this high. With testing being so difficult to obtain for the asymptomatic as it is, let alone inmates, my suspicion has been that anyone who is being reported as infected, is sick. And based on typical BOP response to inmate illness, that they are very sick. But maybe they’ve stepped up.
Do you have any sense of how widely they are testing? If they are testing asymptomatic staff or inmates?
From what I can see, the response has been piecemeal. Seatac FDC shut down visitation on Fed 28, when Inslee declared Washington to be in a state of emergency. It was at least a week before I saw another prison do the same and a similar space of time before the whole system finally did. The Director of Prisons says they began to meet about the virus in late January, and that they have plans in place for epidemics. I’m skeptical about whether they have been any more proactive than anyone else in the government but would love to learn otherwise. Its very hard to tell if they have sequestered new inmates and transfers from existing populations. As for early releases, I read a report of an inmates family member, that they are sequestering the inmates selected to go early for two weeks, but in adjacent cells in SHU to inmates who have tested positive and are presumably sick. Also that early release for many people means being sent to half way houses and the like, which are as problematic as the jails.
As you said, the worst fear is about local jails. There are still regions where good old boys are laughing at this, and good old boys run a lot of jails. I forget which county or state jurisdiction it was last summer, where they didn’t evacuate subterranean cells in a prison that was directly in a hurricane path, the inmates ended up treading water with a couple ft. of headspace left, like in some cliffhanging thriller, but that is the standard of care I worry about. Also, understaffing is already so rampant, that its easy to picture bedlam breaking out as staff get sick, or because they simply flee their $7.40 an hour CO jobs, en masse, either in terror of the virus, or riots. Ugh.
The Oakdale outbreak was always one of the big ones, so any list that didn’t include that was incomplete. As I tried to note, from both Oakdale and Elkton, the numbers hospitalized with symptoms are significantly higher than those who’ve been tested positive, and that’s just symptomatic people (which is a lousy way to try to beat an epidemic in a closed space).
Click through to the links RE BOP’s release policy and Barr’s action–per a series of Josh Gerstein articles, they did impose that 2-week quarantine but have since waived it.
I have reason to believe that Trump is trying to convince us all of something that is truly bat guano insane; namely, that saving lives supposedly also leads to death (…) albeit, a different form of death.
That’s a paraphrase of Trump’s blather the other day about the upcoming most important decision in his life.
https://www.archyde.com/trump-decision-to-reopen-economy-will-be-the-most-important-in-my-life/
2 days ago … “Staying at home also leads to death (…) Perhaps a different form of death,” he said.
Assuming that The Governors’ stay-at-home orders are currently saving lives, you should be able to derive the crazy paraphrase from the Trump quote cited above.
But then there’s also the “bridge too far” effect to consider. If saving lives leads to death, then why wouldn’t causing death lead to saving lives (…) Perhaps a different form of life??
Does there remain anything TOO CRAZY for (. . . ) The Chosen One??
The formulation is very common among Freakonomics style hack economists who like to draw correlations between the number of takeout meals consumed in Chicago and outbreaks of civil war in Central Asia.
They’re just doing endless P Hacking, searching through giant data sets to find coincidental occurances, but they are really common among the shouty set of economists that surround Larry Kudlow.
There has been some really nasty sniping by some of these types of economists at epidemiologists during the pandemic. Richard Epstein wrote a piece for the Hoover Institute that was widely circulated in the White House in the beginning of the year that attacked forecasts and said deaths would top out around 500 and the costs of strict measures were terrible.
https://www.newyorker.com/news/q-and-a/the-contrarian-coronavirus-theory-that-informed-the-trump-administration
Epstein also based his ideas on a completely wrong understanding of evolution, which is another common trait of a lot of these awful hacks.
Thanks Bob. I should’ve known that I had bitten of more than I could chew when I asserted that “Trump is trying to convince us all of something . . . [anything].”
If Trump is so keen on starting things up again, I’d suggest he and his republicans lead by e.g. Let them go out and ride subways, go into the prisons nursing homes, naval ships, etc. If its good enough for the citizens of the country it ought to be good enough for trump and his family and administration. sOh, they won’t go, well then neither should the rest of the country. Not until the people of the country can be supplied with the necessary protective equipment and testing should things open up again. People go to work, aquire the virus, come home give it to their families and their families die. well that isnt’ worth it, unless of course trump and his administration are willing to have some of their family members die in aid of opening the economy
Of course, this line is kin to the thought that top politicians’ shouldn’t be able to keep their sons (and daughters) from the harm propelling a war imposes on the less blest.
It is mentioned above on transmission of Covid-19 comparing the MV Diamond Princess to the USS Theodore Roosevelt, that sailors would be better able to maintain the discipline of social distancing.
(Rummaging through my seabag to put my Dixie cup back on from my carrier days): Nope, that is not possible. Social distancing is not possible in berthing compartments with a hundred people in them with racks (beds for landlubbers) stacked three-high, or working in enclosed spaces whether a maintenance shop, bridge, or engineering space.
Any ship the virus gets aboard, it will rapidly spread. Even on an aircraft carrier with a (relatively) large sickbay, quarantine is extremely limited; the best way to quarantine is to get the infected person off the ship. That is possible on ships which can accept aircraft; for those which can’t, they have to be transferred to a ship which can fly them out (risking spreading the virus to that ship), or mooring at a pier or anchoring out and transporting them ashore.
Sure, but those berthing compartments are what cruise ship WORKERS work in, and they bring food to the passengers who’re quarantining in closed rooms.
All I meant with the discipline issue is that sailors have already been trained for survival under certain situations and trained to take orders. Old rich cruise ship passengers are less likely to be good at that.
I understood what you meant with cruise ships.
It is impossible on a Naval vessel to socially distance. Not at work, not at chow (or in the chow line, where galley workers directly handle your food and hand it to you), not in the head (bathroom), not in the rack.
I don’t recall in seventeen years of Naval service where I ever could have put more than a couple feet between me and anyone else as an avionics technician working on equipment in a shop.
It was reported the USS Theodore Roosevelt first had its outbreak in the Reactor Department (that is, the nuclear reactor engineering spaces).
It would even be worse on submarines, where sailors actually share racks between shifts.
Agree. One thing that has been remarkably underreported is that another ship in the Roosevelt’s carrier group had an outbreak too.
The Navy has an unbelievable challenge on its hands. Still, I’m puzzling through the 12% (as compared to the cruise ships 16-19%). I’m wondering if the difference is just age and better health, or whether the Navy managed to do something better than the cruise ships?
I can’t say why the difference in reporting.
That said, the French aircraft carrier Charles De Gaulle just reported they have fifty cases.
https://www.europe1.fr/societe/covid-19-a-bord-du-charles-de-gaulle-les-marins-qui-nont-pas-respecte-les-regles-doivent-etre-sanctionnes-3961696 (in French)
Yikes.
It’s, as you say, a nearly impossible effort to try to keep ships safe. And as you saw, there have to be submarines with far worse problems.
The map that Will Arkin liberated shows cases by bases. But those San Diego and Norfolk cases might be for ships that are based there, not sailors on base.
Correct me if I am wrong, but it is my understanding that under the same circumstances an older person is not more susceptible to CATCHING the virus than a younger one?
Testing data from Iceland (which tests widely, both symptomatic and asymptomatic persons) and Netherlands (which tests symptomatic for COVID-19) show that younger persons are more likely to catch the virus — they just aren’t as likely to be symptomatic resulting in severe to critical cases requiring hospitalization.
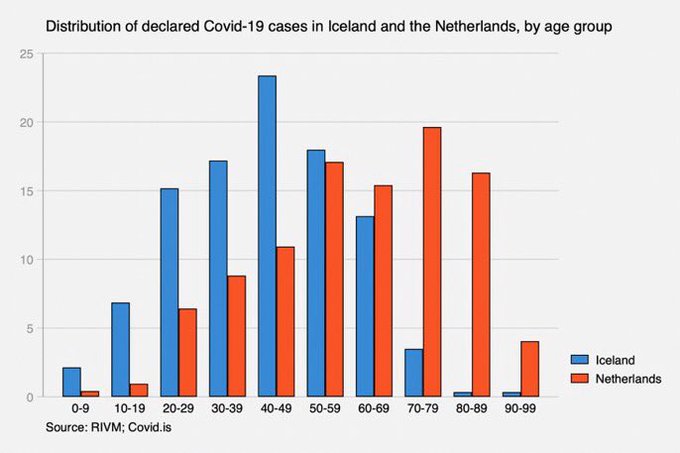
Here in Austin, many more younger people than older people aren’t observing social distancing, which could account for why more younger people are getting infected.
The biggest driver behind younger people not observing distancing is poorly disseminated explanations of findings to date about the virus. The data from China was construed incorrectly to mean young people aren’t affected by the virus while older and immune-compromised were more at risk.
We simply don’t know that. We can’t say with certainty there isn’t sequelae among young people who have been exposed. This wretchedly awful administration made zero effort to ensure young people understood what we didn’t and still don’t know about the virus.
And frankly, younger people are in school and at work in closer proximity. They were already close to begin with around the globe. They may yet pay a price for proximity now whether their choice or ours by failing to protect them sooner.
I think we have a lot of clues but I’m not sure we know for sure if it’s the lifestyle difference between juniors and seniors that would give the virus an easier chance of hooking the younger ones.
As for the lower stats on the Navy vs cruise ships, I wonder if it’s as simple as “military” cleanliness and minimalist surroundings?
I’m not going to touch the age issue because the data we have can be sliced and diced; there are some differences between locations/cultures when same data types are compared.
As for the “military” cleanliness: cruise ships are run for-profit and not configured for military service. They are fundamentally different in construction as well as operation, like comparing residential to business buildings. This is really not suited for comparison. It’s more important to compare like to like: why haven’t northern cruises had the same level of contagion as subtropic/tropic cruises? Why do cruise ships have so many outbreaks like norovirus and does norovirus also affect northern as well as subtropic/tropic cruises? What is it about cruise ships’ business model which fails to prevent the spread of infection, no matter the virus?
In an early report of the Diamond Princess, ( 531 positives instead of over 700), 43 of 776 persons between 20 and 39 tested positive. https://www.niid.go.jp/niid/en/2019-ncov-e/9407-covid-dp-fe-01.html
Hey, James & Marcy – My 2 cents, fwiw:
Having worked in a non-essential service on 3 different bases (2 air stations, 1 sub) and in local government under several administrations, I was routinely required to accumulate and analyze usage statistics. In my experience, these statistics were always subject to the egos of higher level officials.
For me, it took a couple of times of being called on the carpet for representing the facts before I learned not even to ask how high to jump the next time. Some “superiors” were decent people with reasonable egos. Others might have been fully compliant for their own bosses (who might have been malignant narcissists, or just “following orders” as the monsters at the Nuremberg trials were wont to say…)
So, “lies, damn lies, and statistics” as the misattributed phrase goes. My bet is that the facts will be slippery for a long time, maybe forever.
One place the federal government is tracking and releasing data is in VA facilities. VA is separate from DOD active military, but clearly connects with them. Military Times has been watching this, and their latest update (from Friday) is here:
I’ve had my eye on that but using VA numbers is really tough because of the demographic diversity that could include. Their deaths might just be old Vietnam veterans whose neighbors are also dying in large numbers, or it could represent people in VA facilities, representing nursing home-type clusters.
The employee numbers would seem to suggest these are mostly VA hospital-specific, rather than general community contagion.
It seems that Trump’s need to hide reality is contagious. Eugene Scalia, Sec’y of Labor, has decided that most businesses do not need to track Covid-19 cases among their employees – because it would be too much of a burden on them, dear things.
Eugene Scalia, of course, is the son of Antonin Scalia and a famously anti-labor lawyer and lobbyist, and a longtime GOP fixer. His department’s OSHA issued guidelines that would allow the non-reporting of a “recordable illness.”
Apart from gaming the incidence, location, and spread of a dangerous global disease – which seems to protect Trump’s fragile ego and re-election prospects – the move would seem to reduce costs to business. Such delicate things are free-standing, independent-from-government, boot-strapped capitalist enterprises.
https://www.rawstory.com/2020/04/former-osha-officials-sound-alarm-as-trump-tells-corporations-they-dont-have-to-record-coronavirus-cases-among-their-workers/
Seems to me that tracking cases by the employer would help them *lower* costs. Is someone out for a day with a cold, or out for the foreseeable future with COVID-19? Is a cold going around my business or COVID-19? The answers to questions like these make a big difference to an employer. Do they need to simply rearrange duties for a day or two among healthy workers, do they need to hire temps to replace folks out for longer periods, do they need to take massive steps to clean potentially contaminated spaces, do they need to take additional steps to socially distance, do they need to consider shutting down completely?
If you don’t track cases, you can’t answer these questions — and that could be a VERY expensive gap in an employer’s knowledge.
I think your observation is accurate But it does conflict with both “employees are the enemy” and “all employees are fungible” mantras. Large-scale employers also seem to consider their customers fungible, so that the absence of a few is something easily replaced.
Social pathology among business leaders is not new. Past examples include the Robber Barons, bankers generally, and the Ford executives who decided not to re-engineer the Ford Pinto gas tank because it was cheaper to pay personal injury claims instead. But it seems more highly regarded and rewarded in neoliberal America. Another good reason to prohibit or tightly regulate private business participation in providing health care.
The classic Sam’s Club vs Costco approach to employees. Do you treat them as cheap widgets and easily replaceable so you get them as cheaply as possible, or do you treat them as valuable and worth holding onto so you pay them more?
Per Harvard Business Review in Dec 2006, the numbers say Costco has it right. From their conclusion:
In the midst of an epidemic and in its aftermath, the rate of employee turnover (regardless of whether it is for financial or medical reasons) will be a very very important metric to watch. Those businesses with lower turnover rates will likely be the fastest to make the changes needed to deal with the effects of the epidemic as well as those most ready to move fast when things begin to open up.
it is nothing more than an old, though very strong, social convention in our society that the “owners” of a corporation, or managers acting for them, should get to decide how the income and profits are divided among all persons working for the organization. inevitably they favor themselves with the weight of societal approval supporting them.
it is entirely conceivable to have a corporation (and a society of corporations) that divides income up very differently from koch industries or liberty media, where 100’s of millions of annual reward each go to a few high-level officials and a relative pittance is paid out to the rank-and-file.
it is conceivable to have a not-for-profit corporate culture where business corporations prosper but extreme wealth-collecting is not sanctioned or tolerated by society. those who are talented at managing others can lead and be appreciated for their skills, but willl not be excessively compensated relative to other employees.
a central requirement for this different way of rewarding work and status is to openly and legally acknowledge the obvious, that corporations cannot operate without their workers’ energy and intelligence. the organization’s leaders (ceo,coo,cfo 😄) have a specialized job to do, but then so do the other workers. take those workers away and there is nothing to manage and no product or service available for sale. the scale of just and fair compensation needs to operate without the weight of the thumb of bias in favor of those who own or manage the organization.
among other matters, this would require getting rid of the “financialization” of american corporations in which the entire organization is treated as an entity to be bought, sold, bartered, or traded by, e.g., private equity groups and hedge funds. it would also require disconnnecting wall street influence from individual corporate decision making.
the changes needed are in our society’s values, not in our society’s corporations’ structure or management.
Our state AG is investigating a cluster amid residents and staff at a local nursing home. Six deaths and 50 positive. He is looking into adequacy of protective measures and internal controls. The home is trying to blame outside workers who come in to help residents, such as therapists and beauticians.
Never mind that the home sets the rules and policies about which therapists and beauticians can come in, and the circumstances under which they do their work while at the home.
They might want to come up with a better response when the AG’s team comes to visit, because that one won’t work.
Marcy, Great post (as always) but especially relevant to me. I am the medical director of an 80 bed nursing home in coastal NC that serves a large under-served population (poor, homeless and mentally ill people). I have been on the frontlines of this issue since January (when we started to hear preliminary reports from China) and started to worry about our vulnerable population. Since then, everyone (staff and residents) has their temperature taken daily and we all wear surgical masks to protect others from us. We are not allowing any visitors and only essential hospital visits (like going to dialysis) are permitted.
Besides the obvious issues of housing numerous frail, highly vulnerable people with comorbidities there are also subtle problems in long-term care. For example if someone requires transfer to the local hospital ER, they must be quarantined for two weeks when they return. Another concern is the high false negative rate of hospital Covid screening in our area. The test sensitivity is between 70 and 80% so a negative test is not totally reassuring. We just admitted a man to our facility with pneumonia and a negative Covid test screen that I worry about. If I decide to retest him the turn around time for the test result is over 2 weeks from our local health department. Frankly I worry that hospitals may be minimizing testing on potential nursing home transfers to simplify the process and avoid hassles. PPE is also a real issue. So far we have dodged two known bullets and have no cases in our facility. However this is a major undertaking for our team, especially since our local community is not yet at its peak of infections.
Another data point. April 13, Oregon reports 321 hospitalized Patients with suspected or confirmed COVID-19, 145 Only patients with confirmed COVID-19. Not reported is how many results pending or likely false negatives. https://govstatus.egov.com/OR-OHA-COVID-19
I’m not sure where to put this, but thought it might be of interest, from Wendy Siegelman:
https://twitter.com/WendySiegelman/status/1249727748253286403
11:54 AM · Apr 13, 2020
No bankrupt small homeowner ever had as many debts to pay as Jared Kushner and Donald Trump.
Suspect we will hear more about R soon. One paper estimated R in Wuhan as 0.32 from Feb 2 to Feb 11. And 8 weeks later Wuhan is slowly unlocking. Simplified an R of the square root of 0.32 takes twice as long to reduce the number of infectious people as 0.32. R will be larger for a while as cases in isolation infect their close contacts. Seems to me looking at Washington state there is quite a ways to go. https://www.livescience.com/can-covid-19-be-crushed.html
Out of general interest on hydrocloroquine and ACE, there is a summary of recent findings circulating on Facebook written by Pierre Sonveaux (PS) from UCLouvain (Belgium) discussing the following papers
(1) The host’s angiotensin-converting enzyme polymorphism may explain epidemiological findings in COVID-19 infections. Delanghe JR et al. Clin Chim Acta 2020 :505 :192-193.
(2) https://www.ugent.be/nl/actueel/corona-polymorfismen
(3) Chloroquine is a potent inhibitor of SARScoronavisus infection and spread. Vincent MJ et al. Virology Journal 2005;2:69.
It says among other things (which are compatible with the Quinn Norton (QN) post on the topic)
—A high level of ACE means a higher susceptibility of infection…but a lower risk of death, because ACE regulates the inflammation of the heart /cardiovascular diseases. The more there is the less the cytokine storm is likely to happen.
—Polymorphism of the ACE means some populations are genetically less susceptible of being infected, such as Northern Europeans and Slavs, because the geometry of the ACE is different (virus has the wrong key for lock using the metaphor used by QN and PS).
—Hydroxychoroquine and chloroquine modify the geometry of the ACE, but also inhibits it, therefore leading to heart failure at times. So it can be useful in some cases, and deadly in other..
Monroe Correctional Complex (one of 4 complexes side by side) in Washington State had a “riot” on April 9, after 9 inmates were found to be positive. The disturbance was in the exercise yard which is the size of a couple football fields. It sounds more like civil disobedience meant to draw public attention to their plight, than what we traditionally think of as a riot.
Another off topic item people may be interested in:
https://twitter.com/ScottGottliebMD/status/1249873227939266560
9:32 PM · Apr 13, 2020
Links to:
Universal Screening for SARS-CoV-2 in Women Admitted for Delivery
https://www.nejm.org/doi/full/10.1056/NEJMc2009316
April 13, 2020 DOI: 10.1056/NEJMc2009316
Marcy on Slavitt re best practices vs. poorer ones, and your comment here (albiet from a completely different angle) each remind me of this story. By implication these are float nurses, tasked with moving from ward to ward within shifts:
Anguished nurses say Scranton hospital risked infecting cancer patients, babies and staff with COVID-19
https://www.inquirer.com/health/coronavirus/coronavirus-covid-scranton-pennsylvania-hospital-endangered-staff-patients-20200411.html
this washington post report by josh rogin suggests a source of the sars-cov-2 virus, an extremely high-level virology lab in wuhan that may not have been adequately manned or well-managed. this initial observation was by abu.s. state department expert team visiting the lab.
“… most importantly,” the cable states, “the researchers also showed that various SARS-like coronaviruses can interact with ACE2, the human receptor identified for SARS-coronavirus. This finding strongly suggests that SARS-like coronaviruses from bats can be transmitted to humans to cause SARS-like diseases. From a public health perspective, this makes the continued surveillance of SARS-like coronaviruses in bats and study of the animal-human interface critical to future emerging coronavirus outbreak prediction and prevention.”
The research was designed to prevent the next SARS-like pandemic by anticipating how it might emerge. But even in 2015, other scientists questioned whether Shi’s team was taking unnecessary risks. In October 2014, the U.S. government had imposed a moratorium on funding of any research that makes a virus more deadly or contagious, known as “gain-of-function” experiments.
As many have pointed out, there is no evidence that the virus now plaguing the world was engineered; scientists largely agree it came from animals. But that is not the same as saying it didn’t come from the the lab …”
“…this story is not about blame…”
https://www.washingtonpost.com/opinions/2020/04/14/state-department-cables-warned-safety-issues-wuhan-lab-studying-bat-coronaviruses/
Since all of these essential workers either have been, will be, or should be wearing masks for extended periods — ones that hurt the ears — I’m sticking this comment here about mask holders: tricks and devices to hold the straps so your ears don’t have to. Everyone has different workplace uniform, safety, and other occupational standards, so some/all may be Not Applicable, though us regulars might enjoy some of these modes of relief during our brief excursions.
Some weeks ago I had mentioned headbands with buttons so the straps could attach to the buttons. Those evolved into a single button in the back of the head (easier to make). People with long hair can attach the straps to a bun(s). Others rig the straps around a paper clip, or string of them, at the back of the head (and some use paper clips to attach them to surgical caps, even the paper ones that are like hair nets — which a lot of workers wear — or a button sewn to fabric headgear).
But the greatest thing since sliced bread — made a *world* of difference in local mask-wearer’s quality of life — are the 3-D printed mask-strap holders, as they allow for ~sizing.
This is a just-updated version closest to what he received (THANK YOU, LOCAL 3-D PRINTER):
Ear Saver Strap Extension V2 (Surgical Mask Tension Release Band) | NIH 3D Print Exchange
https://3dprint.nih.gov/discover/3dpx-013840
You can see other variants on the main page by clicking the “NIH 3D Print Exchange” link at top left.
[And looking at them gives ideas perhaps for other things that might be repurposed.]
If I had a 3-D printer, I’d be cranking these out.
MICHIGANDERS:
https://twitter.com/kylegriffin1/status/1250061244993691648
10:00 AM · Apr 14, 2020
Trump threatens “Democrat Governors”:
https://twitter.com/realDonaldTrump/status/1250075668282576898
10:57 AM · Apr 14, 2020
Movie. Because he can’t read a book.